J Biomed 2017; 2:20-24. doi:10.7150/jbm.17864 This volume Cite
Review
Advanced Perfusion Techniques - Flow versus Pressure
1. Cardiac Surgery Department, 401 Military Hospital, Athens, Greece;
2. Thoracic Surgery Department, “Theagenio” Cancer Hospital, Thessaloniki, Greece;
3. Pathology Department, “Theagenio” Cancer Hospital, Thessaloniki, Greece;
4. Department of Nursing, School of Health Sciences, Cyprus University of Technology, Limassol, Cyprus;
5. Pulmonary Department-Oncology Unit, “G. Papanikolaou” General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece;
6. Surgery Department (NHS), University General Hospital of Alexandroupolis, Alexandroupolis, Greece;
7. Ear, Nose and Throat Department, “Saint Luke” Private Hospital, Panorama, Thessaloniki, Greece;
8. Department of Anatomy, Democritus University of Thrace, Alexandroupolis, Greece.
Received 2016-10-10; Accepted 2016-11-2; Published 2017-1-1
Abstract
Cardiac operations which require Cardiopulmonary bypass (CPB) are considered the most common procedures in cardiac surgery, performed for more than half a century, especially in Europe and North America. Despite that new technologies are being incorporated in CPB as long as the development of new techniques in CPB, some debates still remain. These debates regard the achievement of the needed optimal perfusion during CPB and the relation between perfusion pressures and the optimal blood flow during extracorporeal circulation. Blood flow and blood pressure during Cardiopulmonary bypass are very important factors. Although more studies are in favor of a minor superiority of the optimal blood flow requirements, compared to the corresponding optimal blood pressure needs, their role is quite interdependent. The usage of contemporary electronic Data Management Systems (DMS) led to a significant evolution of the perfusion science. Adequate perfusion can now be judged by its results in real time, while information from DMS, such as venous saturation, levels of haemoglobin and lactate, may be used as the markers of optimal perfusion and additionally for the development of the perfusion protocols in the future.
Keywords: Cardiopulmonary bypass, blood, flow, pressure.
Introduction
Cardiopulmonary bypass (CPB) has been used widely with success in cardiac surgery for more than half a century.[1] Despite the new technologies that are being incorporated in CBP involving new pumps, new blood gas exchange devices, new centrifugal heads, miniaturized CPB, and of course, the development of the perfusion training programs mainly during the past 30 years, which led to the scientific evolution of perfusionists and to the development of new techniques in CBP, some debates still remain. These debates are usually related with the ways of achieving the optimal perfusion during CPB and mainly with the relation between perfusion pressures and the optimal blood flow during extracorporeal circulation.
Blood Flow and Blood Pressure: An Interactive relationship
The study of the two above factors is even more difficult because the changes in the conditions that one patient is submitted have as result changes in the need for perfusion flow or blood pressure. Perhaps the most obvious example is changes in body temperature. Low blood flow and low blood pressure during hypothermic CPB has been accomplished with good clinical outcome without mentioning that every patient corresponds differently to CBP (CPB).[1] This is a reason that can explain why cardiac centers differ their protocols regarding to what the optimal blood flow or blood pressure should be during CPB.[2] However, the optimal perfusion should be defined by the outcome on the patient and particularly in terms of brain, kidney, gut function along with optimum respiratory function.[1]
The relationship between blood flow and blood pressure can be described by the relationship: F=ΔP/R, where F is the blood flow, ΔP is the perfusion pressure, which is the pressure difference between two points of a blood vessel or an organ, and R is the resistance to flow across this blood vessel or organ. This equation refers to laminar flow and indicates that there is a proportionate relationship between pressure and flow.[3] However, when conducting a CPB, perfusion pressure and blood flow are independent factors.[4]
Blood Flow during CPB: Goals and Requirements
One of the main goals, if not the greatest, when conducting CPB is the delivery of oxygen to the tissues. This is dependent on two individual parameters, the blood flow and the O2 content of the arterial blood (CaO2). Therefore, adequate blood flow must be delivered throughout the conduction of CPB.[5] The blood flow that is required in order to result in adequate perfusion of the tissues is determined by several factors such as the Body Surface Area (BSA) of the patient, the acid-base balance, the degree of hypothermia and the depth of anaesthesia.[1] A fixed arterial blood flow depending on BSA was proven to be safe but it resulted in hyperperfusion during hypothermia.[6] Thomassen and colleagues came to the conclusion that an extensive range of blood flows from 1.9 to 3.1 L/min/m2 have the ability to preserve adequate systemic and cerebral oxygenation.[7]
Global oxygen delivery (DO2), which is the amount of oxygen delivered to the body, has a proportionate relationship with cardiac output (CO), which actually is the blood flow, and with CaO2 and is given by the equation:
DO2 = CO x CaO2.
Furthermore, CaO2 also has a proportionate relationship with haemoglobin.[8]
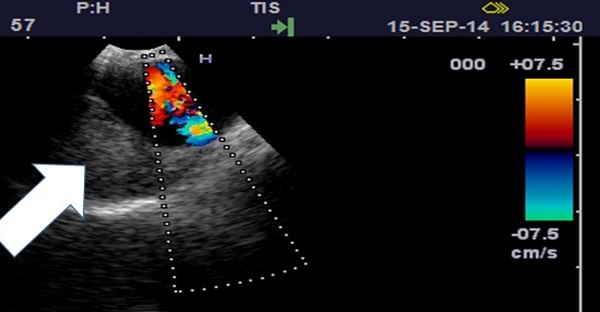
In a study that was published in 2013 which points the influence of the variations in blood flow and pressure on systemic and cerebral oxygen saturation during CPB found that the maintenance of flow and thus DO2 was more important than the maintenance of mean arterial pressure (MAP).[9] In the same study, a phenylephrine-induced increase in MAP led to the decrease of cerebral oxygen saturation (Sco2) and thus to the DO2 to the brain. Bennett and his colleagues came to the conclusion that in conventional CPB, the reason for cerebral desaturation was the failure to achieve the target of the blood flow rate.[10] In the same study, when using mini-CPB, the most important parameter was the haemoglobin concentration. Furthermore, a major complication that is associated with cerebral hypoperfusion is the postoperative cognitive decline (POCD) after CPB.[11] Using continuous transracial Doppler ultrasound Messerotti Benvenuti et al found that reduced cerebral blood flow (CBF) velocity in the left main cerebral artery was related with POCD three months after cardiac surgery and the results were independent of the EuroScore or the educational status of the patients. CBF velocity in the right MCA was not related to POCD.[12] Blood flow and blood velocity according to Poiseuille's law have a proportionate relationship given by the equation:
F = V x A
F=flow, V=mean velocity and A= cross-sectional area of the vessel.[3]
Adequate blood flow during CPB is also important for the kidney especially during rewarming phase when the medullar oxygen consumption is high. This is the phase when the kidney is more susceptible to hypoxic damage.[13] In a previous study renal blood flow was superiorly influenced by the pump blood flow while the arterial pressure was of inferior significance.[14] In addition to this study Azau and colleagues showed that an increased beset arterial pressure during CPB did not decrease the prevalence of acute kidney injury (AKI).[15]
In a retrospective analysis that was published in 2008 that analyzed risk factors of gastrointestinal complications after cardiac surgeries, found that the decrease in blood flow and thus DO2 results in a state that the GI tract is not capable to recompense, because it doesn't have the ability of autoregulation.[16] Furthermore this state of hypoperfusion might be continued even after the re-establishment of adequate flows and pressures. A study that compared the importance of flow versus pressure during CPB in rabbits using laser Doppler flowmetry showed that the low splanchnic perfusion during CPB in mainly reliant on the pump blood flow.[2] Perfusion pressure was of secondary importance. Furthermore, Adluri and his colleagues found that the reduced hepatic blood flow when commencing CPB can be balanced by an increase of the pump flow rate by 20%.[17] For their study they used the indocyanine green method which measured its percentage dye, and therefore overwhelmed the difficulty of the dual blood supply to the liver. In addition, reduction of blood flow through the splanchnic circulation cause to endotoxemia as it may end to the failure of the mucosal barrier in the GI tract.[18]
Blood Pressure during CPB: Role and Particularities
The definition of the ideal systemic blood pressure during CPB is yet to be defined. All the previous studies that pointed the importance of blood flow do not eliminate the importance of MAP.[9] In every study MAP was kept above the level of 50mmHg excluding periods when there was a surgeon request or unwanted quick falls. Consequently, differences in MAP and the importance that those differences have, can only be compared between the range of 50 and 60mmHg, which is considered as the lower limit of a generally accepted of safe perfusion, and 70 and 80mmHg.[1]
The role of a high MAP in the protection of the brain was described among others by Plestis and Gold. They found that a high MAP would be highly recommended for the protection of the brain and the abdominal organs especially for patients with high risk of embolization.[19] That would actually be and the most obvious practice during CPB. An increase in the MAP and the maintenance of a higher blood pressure would reimburse the drop of the pressure across the stenosis[20]. This is a common practice with patients with carotid stenosis. Furthermore a number of studies support that cerebral blood flow and thus cerebral oxygenation is mainly related to the perfusion pressure and not to the flow rate during CPB.[21] An increase in MAP doesn't imply that it will lead to an increase in the cerebral arteries resistance as it is very susceptible to PaCO2 changes and vasoconstrictors that are largely used in CPB, such as phenylephrine, that increase MAP, do not pass the blood-brain barrier.[22, 23]
Systemic blood pressure has also a major role in the maintenance of the renal function. When MAP drops below the optimal autoregulation threshold the renal blood flow is decreased.[24] Furthermore, the more time MAP is below 50mmHg or 60mmHg during CPB, the more likely is for acute renal injury (AKI) to arise.[25, 26] Kanji and colleagues also found that a drop in MAP bigger than 26mmHg during CPB compared to pre-bypass MAP was associated with AKI.[27]
Blood Flow versus Blood Pressure: “Pros and Cons”
The importance of blood flow is not a panacea. Hangrove and colleagues proved that the displayed pump flows differ than the actual flows that a heart lung machine generates when using a roller-pump.[28] In addition CPB shunts, such as arterial filter purge, oxygenator recirculation, blood cardioplegia can significantly decrease the blood flow that is delivered to the patient.[29] An advantage from lower flows would be a possible myocardial protection, clearer surgical field and less embolic delivery.[30] Low flows decrease the inflammatory response to extracorporeal circulation.[31] Conversely, high CBF velocities are associated with complement activation after CPB, higher micro-embolic load and less trauma to red cells. In addition, high flow velocities lead to turbulence flow (increase in Reynolds number) mainly post-stenotic when using pulsatile flow.[32, 33] Furthermore, microcirculatory blood flow seems to be also dependent on blood gases and temperature.[34]
On the other hand, an increase (70-94mmHg) in MAP during CPB didn't prove to be more beneficial for the renal function of patients undergoing CPB compared with groups of patients that had median (60-69) or relatively low (48-59mmHg).[35, 36] In addition, the role of MAP seems to be more important with the present of haemodilution and hypothermia which means the MAP should be evaluated with haemoglobin and temperature.[25]
Another issue of great importance when comparing the importance of blood flow and pressure during CPB is organ autoregulation. Cerebral autoregulation provides satisfactory perfusion of the brain in a range of different MAPs between some limits. Kidneys have also their autoregulation system. However, blood pressure below the cerebral autoregulation limit is associated with AKI and higher morbidity.[37]
The enquiry for the importance of those two factors can become even more complicated when other parameters are taken into account, such as pulsatile or non-pulsatile flow. Tovedal and colleagues found that there is no difference in cerebral oxygenation between these two techniques but MAP was decreased during pulsatile flow.[19] Similar questions might be formed about the importance of blood flow and pressure when using a roller pump, where the output remains constant, or a centrifugal pump where the output fluctuates depending on the peripheral resistance of the vessels. Finally, how would the superiority or the inferiority of pressure towards flow would be proved in cases where the former is mainly generated by the latter and not by vasoconstrictors or vasodilators?
Conclusion
In conclusion, both blood flow and blood pressure are very important factors during CPB and their role is interdependent. Possibly there might be a minor superiority of blood flow as more studies are in favor of this opinion. Furthermore, studies that are in favor of the superiority of blood pressure are much older and the means of blood pressure measuring were not as accurate at that time (where not as much accurate at that time). Nowadays, electronic data management systems (DMS) opens a new era in perfusion science. Adequate perfusion can be judged by its results in real time. Information from DMS and mainly venous saturation and levels of haemoglobin and lactate and can be used as the markers of optimal perfusion and for the development of the perfusion protocols in the future.[38]
Conflict of Interest
The authors declare no conflict of interest.
References
1. Murphy GS, Hessel EA 2nd, Groom RC. Optimal perfusion during cardiopulmonary bypass: an evidence-based approach. Anesthesia and analgesia. 2009;108:1394-417 doi:10.1213/ane.0b013e3181875e2e
2. Bastien O, Piriou V, Aouifi A, Flamens C, Evans R, Lehot JJ. Relative importance of flow versus pressure in splanchnic perfusion during cardiopulmonary bypass in rabbits. Anesthesiology. 2000;92:457-64
3. Westerhof N, Stergiopulos N, Noble M. Snapshots of hemodynamics: An Aid for Clinical Research. New York, NY: Springer. 2010
4. Fernandes P MJ, Cleland A, Walsh G, Mayer R. What is optimal flow using a mini-bypass system? Perfussion. 2010;3:133-7 doi:10.1177/0267659110371557
5. Kay P, Munsch C. Techniques in Extracorporeal Circulation 4th ed. Taylor & Francis. 2004
6. Alston RP, Anderson A, Sanger K. Is body surface area still the best way to determine pump flow rate during cardiopulmonary bypass? Perfusion. 2006;21:139-47
7. Thomassen S, Larsson A, Andreasen J, Bundgaard W, Boegsted M, Rasmussen B. Should blood flow during cardiopulmonary bypass be individualized more than to body surface area? perfussion. 2011;26:45-50
8. Kolyva C, Ghosh A, Tachtsidis I, Highton D, Cooper CE, Smith M. et al. Cytochrome c oxidase response to changes in cerebral oxygen delivery in the adult brain shows higher brain-specificity than haemoglobin. NeuroImage. 2014;85(Pt 1):234-44 doi: 10.1016/j.neuroimage.2013.05.070
9. Vandewiele K, Bove T, De Somer FM, Dujardin D, Vanackere M, De Smet D. et al. The effect of retrograde autologous priming volume on haemodilution and transfusion requirements during cardiac surgery. Interactive cardiovascular and thoracic surgery. 2013;16:778-83 doi:10.1093/icvts/ivt085
10. Bennett MJ, Weatherall M, Webb G, Dudnikov SF, Lloyd CT. The impact of haemodilution and bypass pump flow on cerebral oxygen desaturation during cardiopulmonary bypass-A comparison of two systems of cardiopulmonary bypass. Perfusion. 2015;30:389-94 doi:10.1177/0267659114548256
11. Likosky DS, Caplan LR, Weintraub RM, Hartman GS, Malenka DJ, Ross CS. et al. Intraoperative and postoperative variables associated with strokes following cardiac surgery. The heart surgery forum. 2004;7:E271-6 doi:10.1532/HSF98.20041035
12. Messerotti Benvenuti S, Zanatta P, Valfre C, Polesel E, Palomba D. Preliminary evidence for reduced preoperative cerebral blood flow velocity as a risk factor for cognitive decline three months after cardiac surgery: an extension study. Perfussion. 2012;27:486-92
13. Sgouralis I, Evans RG, Gardiner BS, Smith JA, Fry BC, Layton AT. Renal hemodynamics, function, and oxygenation during cardiac surgery performed on cardiopulmonary bypass: a modeling study. Physiological reports. 2015:3 doi:10.14814/phy2.12260
14. Andersson LG, Bratteby LE, Ekroth R, Hallhagen S, Joachimsson PO, van der Linden J. et al. Renal function during cardiopulmonary bypass: influence of pump flow and systemic blood pressure. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery. 1994;8:597-602
15. Azau A, Markowicz P, Corbeau JJ, Cottineau C, Moreau X, Baufreton C. et al. Increasing mean arterial pressure during cardiac surgery does not reduce the rate of postoperative acute kidney injury. Perfusion. 2014;29:496-504 doi:10.1177/0267659114527331
16. Vassiliou I, Papadakis E, Arkadopoulos N, Theodoraki K, Marinis A, Theodosopoulos T. et al. Gastrointestinal emergencies in cardiac surgery. A retrospective analysis of 3,724 consecutive patients from a single center. Cardiology. 2008;111:94-101 doi:10.1159/000119696
17. Adluri RK, Singh AV, Skoyles J, Hitch T, Robins A, Baker M. et al. Effect of increased pump flow on hepatic blood flow and systemic inflammatory response following on-pump coronary artery bypass grafting. Perfusion. 2010;25:293-303 doi:10.1177/0267659110378843
18. Ghosh S, Falter F, Cook D. Cardiopulmonary bypass. Cambridge: Cambridge University Press. 2012
19. Tovedal T, Thelin S, Lennmyr F. Cerebral oxygen saturation during pulsatile and non-pulsatile cardiopulmonary bypass in patients with carotid stenosis. Perfusion. 2016;31:72-7 doi:10.1177/0267659115586280
20. Tovedal T, Lubberink M, Morell A, Estrada S, Golla SS, Myrdal G. et al. Blood Flow Quantitation by Positron Emission Tomography During Selective Antegrade Cerebral Perfusion. The Annals of thoracic surgery. 2016 doi:10.1016/j.athoracsur.2016.06.029
21. Schwartz AE. Cerebral blood flow is determined by arterial pressure and not bypass flow rate. British journal of anaesthesia. 2014;112:1123. doi:10.1093/bja/aeu178
22. Quarti A, Nardone S, Manfrini F, D'Orfeo F, Genova S, Silvano R. et al. Effect of the adjunct of carbon dioxide during cardiopulmonary bypass on cerebral oxygenation. Perfusion. 2013;28:152-5 doi:10.1177/0267659112464382
23. Lucas SJ, Tzeng YC, Galvin SD, Thomas KN, Ogoh S, Ainslie PN. Influence of changes in blood pressure on cerebral perfusion and oxygenation. Hypertension. 2010;55:698-705 doi:10.1161/HYPERTENSIONAHA.109.146290
24. Persson PB, Ehmke H, Nafz B, Kirchheim HR. Sympathetic modulation of renal autoregulation by carotid occlusion in conscious dogs. The American journal of physiology. 1990;258:F364-70
25. Haase M, Bellomo R, Story D, Letis A, Klemz K, Matalanis G. et al. Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney injury. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 2012;27:153-60 doi:10.1093/ndt/gfr275
26. Fischer UM, Weissenberger WK, Warters RD, Geissler HJ, Allen SJ, Mehlhorn U. Impact of cardiopulmonary bypass management on postcardiac surgery renal function. Perfusion. 2002;17:401-6
27. Kanji HD, Schulze CJ, Hervas-Malo M, Wang P, Ross DB, Zibdawi M. et al. Difference between pre-operative and cardiopulmonary bypass mean arterial pressure is independently associated with early cardiac surgery-associated acute kidney injury. Journal of cardiothoracic surgery. 2010;5:71. doi:10.1186/1749-8090-5-71
28. Hargrove M, O'Donnell A, Aherne T. Differences in displayed pump flow compared to measured flow under varying conditions during simulated cardiopulmonary bypass. Perfusion. 2008;23:227-30 doi:10.1177/0267659108100458
29. Duan X, Ji B, Liu G, Li Q, Liu J, Yu K. et al. Evaluation of shunting flow differences in varied conditions in a simulated adult CPB model during normothermia. Perfusion. 2011;26:207-13 doi:10.1177/0267659110396114
30. Kaplan J. Kaplan's cardiac anesthesia. Philadelphia: Elsevier Saunders. 2006
31. Jonas RaD J. Comprehensive surgical management of congenital heart disease. London: Arnold. 2004
32. Baufreton C, Pinaud F, Corbeau JJ, Chevailler A, Jolivot D, Ter Minassian A. et al. Increased cerebral blood flow velocities assessed by transcranial Doppler examination is associated with complement activation after cardiopulmonary bypass. Perfusion. 2011;26:91-8 doi:10.1177/0267659110392439
33. Piskin S, Serdar Celebi M. Analysis of the effects of different pulsatile inlet profiles on the hemodynamical properties of blood flow in patient specific carotid artery with stenosis. Computers in biology and medicine. 2013;43:717-28 doi:10.1016/j.compbiomed.2013.02.014
34. Boldt J, Knothe C, Zickmann B, Hammermann H, Stertman W, Hempelmann G. Does correction of acidosis influence microcirculatory blood flow during cardiopulmonary bypass? Br J Anaesth. 1993;71:277-81
35. Boldt J, Knothe C, Hammermann H, Stertmann WA, Hempelmann G. Cold or warm start of cardiopulmonary bypass-influence on microcirculatory blood flow. Perfusion. 1994;9:11-8
36. Sirvinskas E, Benetis R, Raliene L, Andrejaitiene J. The influence of mean arterial blood pressure during cardiopulmonary bypass on postoperative renal dysfunction in elderly patients. Perfusion. 2012;27:193-8 doi:10.1177/0267659112436751
37. Ono M, Arnaoutakis GJ, Fine DM, Brady K, Easley RB, Zheng Y. et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Critical care medicine. 2013;41:464-71 doi:10.1097/CCM.0b013e31826ab3a1
38. Poullis M, Palmer K, Al-Rawi O, Johnson I, Ridgeway T. Pressure and oxygen debt on bypass - potential quality markers of perfusion? Perfusion. 2012;27:244-8 doi:10.1177/0267659112439085
Author contact
![]() Corresponding author: Paul Zarogoulidis, M.D, Ph. D. Pulmonary Department-Oncology Unit, “G. Papanikolaou” General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece. Fax: 00302310992424 Mobile: 00306977271974 E-mail: pzarogcom.
Corresponding author: Paul Zarogoulidis, M.D, Ph. D. Pulmonary Department-Oncology Unit, “G. Papanikolaou” General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece. Fax: 00302310992424 Mobile: 00306977271974 E-mail: pzarogcom.